Social Media Posts


Have you ever wondered how the body protects itself from sickness and disease?
The immune system is a complex defense system of the body that works 24/7 to keep you safe from invading germs that can cause sickness or disease.
There are two different responses that the immune system may use to protect you from invading germs.
Humoral immunity protects the body from extracellular (outside the cell) invaders by producing antibodies against them.
Cell-mediated immunity protects the body against intracellular (inside the cell) invaders that have infected the body cells.
Both immune responses protect your body from sickness and disease.
The COVID-19 vaccines contain a genetic code for the spike protein (antigen) that induces an immune response against it.
One of the ways that the COVID-19 vaccine works is by inducing a “humoral response”, which means it causes your body to produce antibodies.
The immune system recognizes the antigen in the vaccine as being 'foreign' and produces antibodies unique to the COVID-19 spike protein, just as it would for a real germ.
These antibody 'packages of protection’ then remember the germ and can defend against it if you were to become exposed to the virus. However, our research is showing that we have the best protection to severe illness in the six months following a dose of the vaccine.
Antibodies are proteins produced in response to a ‘danger’ signal triggered by a unique marker (antigen) on the surface of an invading germ. Each antibody is capable of binding to only one antigen. It's able to do so by containing a specific binding site to the antigen on the invading germ to recognize and inactive it.
After exposure to a germ, antibodies continue to circulate in the blood, providing protection against future exposure. Our research shows that we have the best protection to severe illness in the six months following a vaccine dose.
Antigens are tiny markers found on the surface of invading germs that warn the immune system that something is ‘foreign’ to the body and harmful. Antibodies are produced to recognize and destroy harmful germs that could otherwise cause you to become sick. Other immune cells are also signaled by ‘foreign’ antigens to destroy body cells that have become infected by invading germs.
Antibodies are specialized protective proteins that your immune system makes after vaccination and infection. Antibodies bind to specific protein sites found on foreign invaders like harmful viruses and bacteria and prevent them from infecting your cells. Antibodies produced after vaccination can bind to the SARS-CoV-2 spike protein and prevent COVID-19.
B cells produce specialized protective proteins called 'antibodies'. Antibodies bind to specific protein sites (called antigens) that are found on foreign invaders like harmful viruses and bacteria. Antibodies can prevent infection and recruit other immune cells to destroy infected cells.
Antibodies produced after vaccination against COVID-19 target the spike protein of SARS-CoV-2, preventing viral infection and eliminating infected cells.
T cells help your immune system fight invading bacteria and viruses / invading germs. There are many types of T cells.
Cytotoxic T cells directly bind to and kill infected cells.
Helper T cells provide 'help' to other immune cells. They can secrete chemical messengers called cytokines to support cytotoxic T cells and promote production of antibodies by B cells.
Regulatory T cells help control the immune response to infection.
Antigen-presenting cells (APCs) move through the body seeking out invading germs. Once a danger is detected, APCs educate the immune cells by processing and presenting antigens on their surface for recognition by other immune cells. This creates a targeted immune response against the specific antigen.
In the context of the COVID-19 virus:
APCs engulf the COVID-19 virus, then process the spike protein (antigen) and present an antigen fragment on their surface to inform T and B cells (immune cells) to specifically target the virus.
Memory cells are long-lived immune cells that remember germs from prior infections. They enable the immune system to respond faster and stronger with re-exposure to that germ.
Memory B cells proliferate and produce large amounts of germ-targeting antibodies after re-exposure. Antibody production occurs much faster than after initial infection.
Memory T cells make copies of themselves immediately upon re-exposure to an invading germ and as such respond to the infection more strongly.
Ever wonder how the SARS-CoV-2 virus makes thousands of copies in the body?
Once the virus enters the lungs via respiratory droplets it uses the replication machinery of the cells in your body to make copies of itself. The virus attaches to human cells via its spike protein and then enters the cells where it replicates. Antibodies produced after vaccination target the spike protein and block the virus from attaching to and infecting cells.
Long COVID is of particular concern for adults over the age of 65 who are at a greater risk of persistent COVID-19 symptoms after their initial infection date.
Research is still being done in order to better understand this condition and its variable presentation among individuals.
The ‘Tripledemic’ of COVID-19, influenza and RSV is a real threat to vulnerable populations within the community. Although they are different, they may present quite similar symptoms. We have compiled symptoms for each to help you identify the difference.
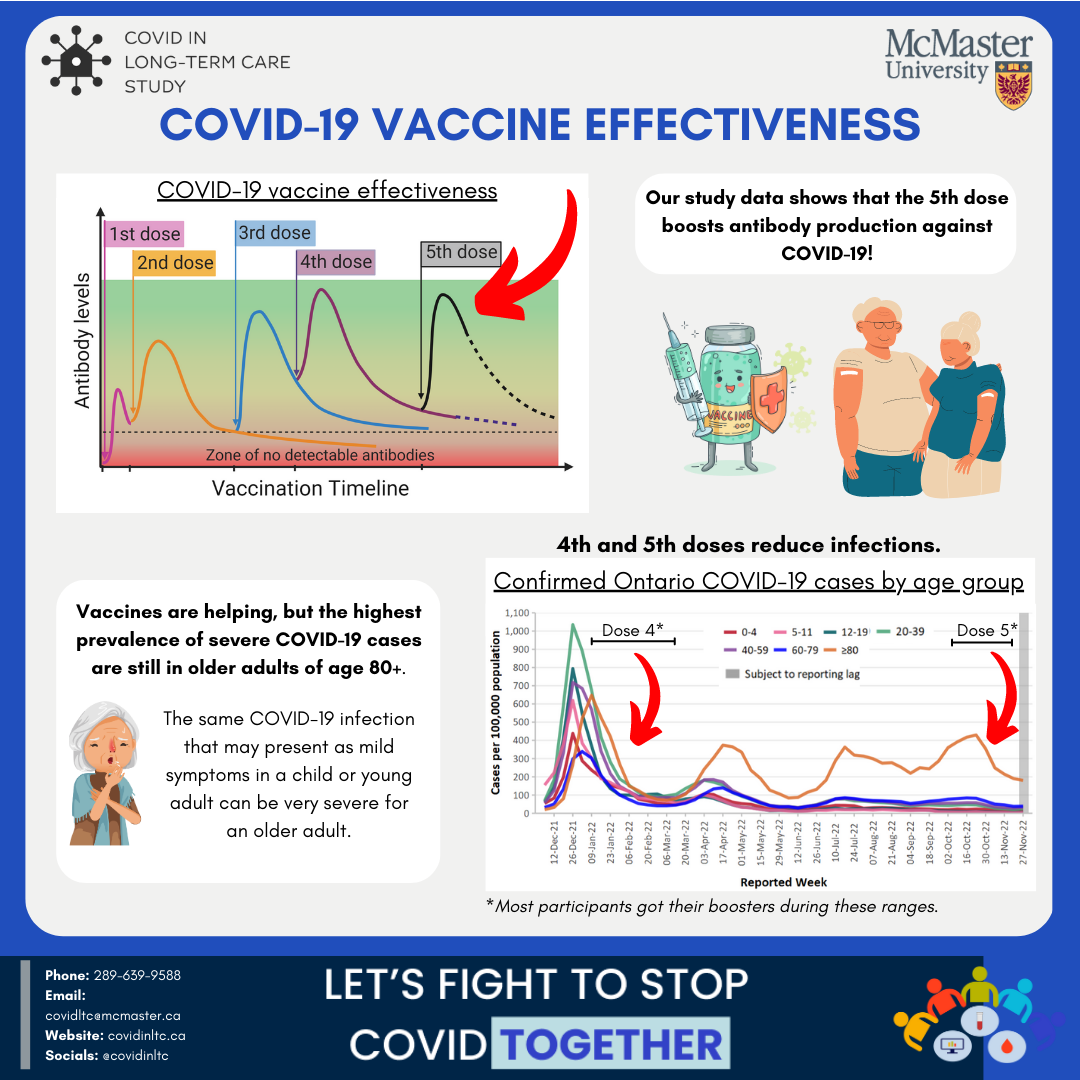
The vaccines are helping, 4th and 5th doses have shown that they reduce COVID-19 infection!
Vaccines are the best way to prepare the immune system for potential exposure to the virus. This means that if you were to become infected, you would not be as contagious or experience as severe symptoms.
With Influenza circulating during the winter months, we wanted to share some information on flu infection and vaccine boosters to prevent infection or co-infection with COVID-19.
Vaccine effectiveness wanes with time, so you are better protected in the weeks following your booster dose than you are several months later. You may be eligible to get an additional booster 3-6 months after your last vaccination or COVID-19 infection.
Antibody levels begin to wane 3-6 months after the last COVID-19 vaccine & 3 months or less after your last COVID-19 infection.
Also, remember that timing the next dose is important! The vaccine needs about 7 days to build up protective immunity.